Are you experiencing joint hypermobility or suspect you may have hypermobile joints? Understanding the complexities of joint hypermobility syndrome is crucial for proper assessment and management. In this article, we delve into the world of hypermobility, exploring its causes, symptoms, and treatment options. Whether you’re seeking answers for yourself or a loved one, this article is worth reading to gain insights into assessing joint hypermobility and managing its symptoms effectively.
A large percentage of physical therapists deal with restricted movement, and when faced with a patient who has good range of movement, there is a danger that it can lead to their condition being misunderstood; which is essentially excessive range of movement within the context of disordered connective tissue. Because of the ubiquitous nature of connective tissue proteins, the possible consequences of tissue trauma are legion. Every patient will need a treatment plan tailored to their particular set of problems.
What Is Joint Hypermobility Syndrome?
Joint hypermobility syndrome (JHS) is a condition characterised by an increased range of motion in one’s joints beyond the normal range. For many, hypermobility does not cause a problem and can even be seen as an asset. For others, their hypermobility brings with it numerous, widespread and longstanding musculo-skeletal symptoms, including pain, which may have been mismanaged in the past. This excessive joint flexibility can lead to various symptoms, including joint pain, stiffness, and instability. Understanding the underlying causes and manifestations of JHS is essential for accurate diagnosis and treatment planning.
Causes and Risk Factors of Joint Hypermobility
Several factors can contribute to joint hypermobility, including genetic predispositions, collagen disorders, and connective tissue abnormalities. Generally, there exists a greater prevalence of Hypermobility Syndrome in females, Asian populations, then Africans and least in Europeans. Joint laxity is usually greatest at birth, decreasing during childhood and continues to decrease during adolescence and adult life. Ligament laxity is determined by the individual’s genetic makeup and hormones, and the genes that encode collagen, elastin and fibrillin are important in influencing joint flexibility. Other factors that impact range of motion include shape of joint surfaces, muscle length and mobility of neural structure. Conditions such as Ehlers-Danlos syndrome and Marfan syndrome are associated with hypermobility and may increase the risk of developing JHS. Understanding these underlying causes can help healthcare professionals tailor treatment plans to address the specific needs of individuals with JHS.
Likely Mechanisms Involved in the Development of Pain Symptoms
- Lack of muscular control in the hypermobile joint range / transferring loads ineffectively and causing subsequent microtrauma to tissues.
- Decreased muscle tone and tensile strength which decreases the overall efficiency in the active support system (Panjabi 1992).
- Less restraint and control offered by inherently weaker ligaments, capsules and fascia leading to a deficiency in the passive support system.
- Deficient proprioception may lead to problems in the neural feedback and feedforward system, leading to abnormal motor control. Individuals with Hypermobility Syndrome have altered proprioception, kinaesthesia, or sense of their body position in space. Therefore, not only is there less support for any given movement offered by the muscles, ligaments, fascia and tendons, there is a reduced ability to sense what is good posture and correct positioning or exercise technique.
Bergmark (1989) proposed there are 2 muscle systems involved in the maintenance of spinal stability;
- Local Muscle System : smaller, deep muscles which attach to the lumbar vertebrae and provide segmental stability and control rather than movement.
- Global Muscle System : large, superficial muscles which directly produce spinal movement without attaching directly to the spine.
There tends to be a cycle of overactivity/underactivity involved with the pain, therefore the individual needs pacing.
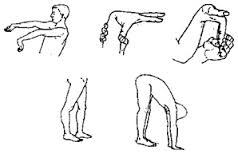
Assessing Joint Hypermobility: The Beighton Score
The Beighton score is a widely used clinical tool for assessing joint hypermobility, involving a series of nine maneuvers to evaluate joint flexibility. Individuals with a high Beighton score may have generalized joint hypermobility, indicating potential underlying hypermobility syndrome. Healthcare professionals rely on the Beighton score to identify hypermobile individuals and guide treatment decisions accordingly.
- (2pt) passively dorsiflex 5th metacarpal joint greater or equal to 90 degrees.
- (2pt) passively flex thumb to wrist.
- (2pt) passively hyperextend elbow greater or equal to 10deg.
- (2pt) passively hyperextend knee greater or equal 10deg.
- Touch palms to floor without bending knees.
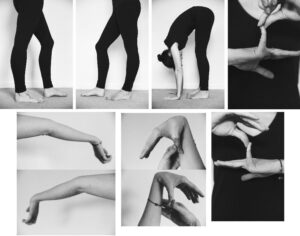
Photographs of real hypermobilty cases can be seen below.
Additional Questions to aid Recognition of Hypermobility Syndrome
- Did they have pain as a child / growing pains?
- Did they participate in Gymnastics or Ballet in their youth?
- Did they feel better or worse in pregnancy? It is common to report a considerable change in their wellbeing during pregnancy (seems that pregnancy was the start of their problems) with more relaxin being produced the joints become more mobile.
- Have they had any dislocations or subluxations or fractures?
- How have they responded to analgesia (usually little effect)?
- Do they dislike sustained postures such as sitting and standing?
- Do they dislike too much activity?
- Do they bruise easily?
- Do they have stretchy skin?
- Do they have any hernia, varicose veins or prolapses (connective tissue is involved systemically)?
- Do they have any neuropathies?
- Do they have Raynaud’s phenomenon?
The Individual Will Often;
- Fidget with hands.
- Have skin that is thinner, stretchier or subject to striae which are not due to large weight changes.
- Have a sway back or kyphosis-lordosis.
- Hyperextend knees.*
- Hyperextend hips (sway back – weak hip flexors, weak glutes).*
- *attempt to gain more stability end-range.
- End-range for passive range of motion testing has a soggy, empty, saggy feel. When resistance is encountered it is often hard and springy, suggesting muscle spasm rather than restriction due to a tight or fibrosed tissue.
- Not all joints are mobile. Eg thoracic and cervicothoracic junction tend to stiffen. These areas have the potential to increase stress on mid cervical and lumbar spine.
- Have increased healing time.
Understanding Hypermobility Spectrum Disorders
Hypermobility spectrum disorders encompass a range of conditions characterized by joint hypermobility and associated symptoms. These may include Ehlers-Danlos syndrome, hypermobile EDS, and hypermobility spectrum disorder. Understanding the nuances of these conditions is essential for accurate diagnosis and tailored treatment approaches to address individual needs effectively.
Managing Symptoms of Joint Hypermobility
Managing symptoms of joint hypermobility involves a multi-faceted approach, focusing on pain management, strengthening exercises, and lifestyle modifications. Physical therapy, occupational therapy, and targeted exercises can help improve posture, muscle balance and endurance, joint stabilisation, proprioception and joint awareness, reducing the risk of complications such as dislocations and chronic pain. Good muscle tone, particularly the deep postural muscles, help protect against injury and improve joint stability. Additionally, adopting a healthy lifestyle and avoiding activities that exacerbate symptoms can enhance overall well-being for individuals with JHS.
Conclusion: Key Takeaways
- Joint hypermobility syndrome is characterized by excessive joint flexibility beyond the normal range of motion.
- Understanding the underlying causes and manifestations of JHS is essential for accurate diagnosis and treatment planning.
- The Beighton score is a clinical tool used to assess joint hypermobility and guide treatment decisions.
- Hypermobility spectrum disorders encompass a range of conditions associated with joint hypermobility and may require tailored treatment approaches.
- Managing symptoms of joint hypermobility involves a multi-faceted approach, including physical therapy, pain management, and lifestyle modifications.
- Treatment options for joint hypermobility syndrome may include physical therapy, splinting, pain management strategies, and, in some cases, surgical interventions.
In summary, assessing joint hypermobility requires a comprehensive understanding of its causes, symptoms, and treatment options. By addressing hypermobility syndrome effectively, individuals can improve joint stability, alleviate symptoms, and enhance their overall quality of life. Whether you’re a healthcare professional or someone affected by JHS, understanding the complexities of this condition is essential for optimal management and well-being.
In ‘Hypermobility’ Part Two, we’ll look at training foundations and progressions.